Definition
Because there is no single anatomic or physiologic characteristic that distinguishes a "child" victim from an
"adult" victim and no scientific evidence that identifies a precise age to initiate Adult rather than Child
CPR techniques, the ECC scientists made a consensus decision for age delineation that is based largely on practical
criteria and ease of teaching. However, American Heart Association's guidelines dictate that Adult CPR is performed
on any person over the age of approximately 10 to 14 years (or post-adolescence, as defined by the presence of secondary
sex characteristics).
Assessing the situation
If you suspect that the victim has sustained spinal or neck injury, do not move or shake him.
1 person CPR
- Verify that the victim is unresponsive by shaking the victim gently and shouting "Are you okay?"
- If there is no response, dial 9-1-1
- Retrieve an AED if one is available
- Begin CPR and use the AED as appropriate
2 person CPR
- Verify that the victim is unresponsive by shaking the victim gently and shouting "Are you okay?"
- A trained rescuer should remain with the victim to begin CPR
- Second rescuer telephones 9-1-1 and, if available, retrieves an AED
- Continue CPR and use the AED as appropriate
Change in CPR Sequence: C-A-B Rather Than A-B-C
Although no published evidence demonstrates that starting CPR with 30 compressions rather than 2 ventilations leads to improved outcome, chest compressions provide vital blood flow to the heart and brain, and studies of out-of-hospital adult cardiac arrest
showed that survival was higher when bystanders made some attempt rather than no attempt to provide CPR.
"C" is for CIRCULATION.
In order to determine if the victim's heart is beating, place two fingertips on his carotid
artery, located in the depression between the windpipe and the neck muscles, and apply slight pressure for several seconds.
If there is no pulse then the victim's heart is not beating, and you will have to perform chest compressions.
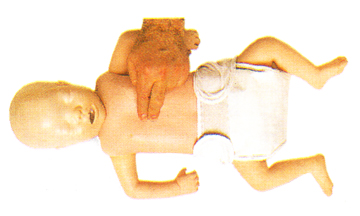
Chest compressions
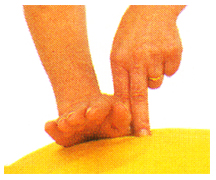
When performing chest compressions, proper hand placement is very important. Place two fingers on the victim's sternum
[
show me] and then put the heel of
your other hand next to your fingers [
show me]. Now you need to place your hand on top of that hand [
show me] and interlace the fingers [
show me].
Lock your elbows and using your body's weight, compress the victim’s chest. The depth of compressions should be
at least 2 inches - remember: 2 hands, 2 inches [
show me] at a rate of
100 compressions per minute.
"A" is for AIRWAY. If the victim is unconscious and is unresponsive, you need to make sure that his airway is clear
of any obstructions.
If you determine that the victim is not breathing, then something may be blocking his air passage. The tongue is the most common
airway obstruction in an unconscious person and it may be necessary to perform a finger sweep in order to move the tongue or
any other foreign object away from the air passage. With the victim lying flat on his back, firmly hold his chin with one
hand while using the finger of your other hand in a sweeping motion
[
show me].
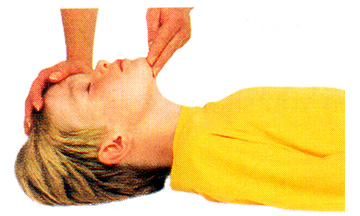
Once the airway is unblocked, place your hand on victim's forehead and your other hand under the tip of the chin
and gently tilt his head backward [
show me].
In this position the weight of the tongue will force it to shift away from the back of the throat, opening the airway.
If the person is still not breathing on his own after the airway has been cleared, you will have to assist him breathing.
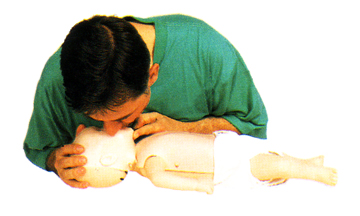
"B" is for BREATHING (skip if performing compression-only CPR). With the victim's airway clear of any obstructions, gently support his chin so as to keep it
lifted up and the head tilted back. Pinch his nose to prevent air from escaping once you begin to ventilate
[
show me].
Take a full breath, place your mouth tightly over the victim's (use a shield barrier if one is available) and blow
[
show me]
until the victim's chest rises. Maintain a tight seal around his mouth and be careful not to over-inflate his lungs as this
may force air into the stomach, causing him to vomit. If this happens, turn the victim's head to the side and sweep any
obstructions out of the mouth before proceeding. Between each breath allow the victim's lungs to relax - place your ear near his mouth and listen for air to escape and watch the chest fall as he exhales [
show me]. If the victim remains unresponsive (no breathing, coughing or moving), check his circulation.
1 person CPR
Count aloud as you compress 30 times at the rate of at least 100/minute. Finish the cycle by giving the victim
2 breaths. This process should be performed 5 times - 30 compressions and 2 breaths - after which remember to check the victim's
carotid artery for pulse (for no longer than 10 seconds) and other signs of consciousness. If you definitely not feel a pulse
within 10 seconds, you should begin cycles of chest compressions and ventilations. Continue until an advanced airway is in place
or victim regains consciousness.
2 person CPR
Count aloud as you compress 30 times at the rate of of at least 100/minute. Finish the cycle by giving the
victim 2 breaths. To prevent fatigue and deterioration in quality and rate of chest compressions the rescuers should change
compressor and ventilator roles every 2 minutes - the switch should be accomplished as quickly as possible to minimize
interruptions in compressions. Continue until an advanced airway is in place or victim regains consciousness.